Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
Keep Your Feet Healthy So You Can Stay Active
Custom Orthotics For Teen Athletes

Parents, support your athletic teens with Custom Orthotics! As they excel in sports and activities, their feet need optimal care. Custom Orthotics provide the right alignment, reducing fatigue and enhancing performance. They help absorb shocks, minimize injuries, and cater to their unique foot structure. Don't let foot discomfort sideline their passion. Invest in their comfort and athletic future by choosing Custom Orthotics from our office. Call today for an appointment.
What Causes Athlete’s Foot?

Athlete's foot is a common fungal infection that affects the skin of the feet, often occurring between the toes. Symptoms include a burning or itchy sensation, scaly, dry, cracked, or peeling skin, blisters on the feet, and sometimes a noticeable odor. This condition is caused by fungi that thrive in warm, moist environments such as shoes, locker rooms, and swimming areas. Athlete's foot can spread easily, if left untreated, leading to discomfort and skin damage. A podiatrist can accurately diagnose the infection, recommend antifungal treatments, and provide guidance on proper foot hygiene and footwear to prevent recurrence. If you have persistent itching, burning, or peeling skin on your feet, it is suggested that you consult a podiatrist who can offer effective treatment solutions, which may include prescribed medication.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
Orthotics and Footwear

When considering orthotics, determining suitable footwear can be perplexing. Orthotics aid in pressure redistribution, and while they are now more versatile due to technological advancements, they are not compatible with all shoe types. Notably, even slim orthotics do not fit well with high heels, suggesting moderation in their use. Ideally, orthotics should be paired with shoes having features like a solid heel counter for enhanced rearfoot support, and a stiff sole for foot stability. Additionally, toe flexibility can enhance easier motion, and a secure front fastening system are also important features. Though many shoe designs fit custom orthotics, some do not due to limited interior space, especially in dress shoes. However, adjustments can sometimes make them fit better. If you are considering wearing custom orthotics and want to know if your shoes are compatible with them, it is suggested that you make an appointment with a podiatrist who can create the orthotics, evaluate your current shoes, and advise you on appropriate footwear.
Custom orthotics can be an important solution for reducing foot pain by targeting its structural causes rather than just the symptoms. When the feet are misaligned, excess strain develops in the muscles, tendons, and ligaments, often resulting in discomfort in the arches, balls of the feet, or toes. Orthotics are designed to match each foot’s natural shape, supporting proper alignment and evenly distributing pressure to ease pain and improve movement.
Foot pain is commonly caused by overuse, wearing improper footwear, or biomechanical issues that place added stress on sensitive areas. By stabilizing the foot and restoring natural motion, custom orthotics help reduce strain, calm inflammation, and promote healing. Many patients experience lasting relief and greater comfort while walking, standing, or exercising.
Created from a detailed assessment using advanced imaging or casting, each pair of orthotics is tailored to your individual needs. If you are experiencing ongoing foot pain, it is suggested that you contact our office for an evaluation and treatment.
If you have any questions, please feel free to contact our office located in Passaic, NJ .
Sole Marketing Supporting Our Feet
The feet form the base of the body’s structure, and proper support is essential for overall comfort and movement. Custom orthotics are designed to give the feet the stability and alignment they need to function at their best. Each pair is created specifically for the shape and movement of an individual’s feet, ensuring that every step is supported and balanced. This personalized fit helps prevent the strain and fatigue that can develop when the feet are not properly aligned.
When the feet lack adequate support, other parts of the body often compensate, leading to pain in the knees, hips, or lower back. Custom orthotics help correct these imbalances by evenly distributing weight and guiding the feet to move naturally. Over time, they can improve posture, reduce discomfort, and make walking or standing more comfortable throughout the day.
Whether used for daily wear, work, or sports, custom orthotics provide consistent support that benefits the entire body.
Types of Diabetic Foot Ulcers
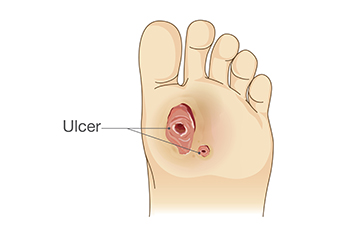
A diabetic foot ulcer is an open sore or wound that develops on the foot due to complications from diabetes. High blood sugar levels can damage nerves and reduce circulation, increasing the risk of ulcers. The three main types are neuropathic ulcers caused by loss of sensation, ischemic ulcers from poor blood flow, and neuroischemic ulcers that combine both problems. Treatment involves cleaning the wound, removing dead tissue, applying specialized dressings, and addressing infection or circulation issues. A podiatrist plays a vital role in managing these ulcers by performing wound care, monitoring healing, recommending protective footwear, and helping prevent recurrence. If you have diabetes and have developed a foot wound, it is suggested that you are under the care of a podiatrist who can determine the type of wound and offer effective treatment solutions.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Foot Corns and Their Causes

A foot corn is a thickened area of skin that forms from repeated friction or pressure, usually on the toes or soles. Symptoms include hardened, raised bumps that may cause pain or tenderness when walking. Common causes are wearing tight shoes, abnormal foot structure, or activities that place excess pressure on certain areas. Risk factors include prolonged standing, ill-fitting footwear, or having foot deformities, such as hammertoes or bunions. A podiatrist can identify the underlying cause, safely remove the corn, and provide custom padding or custom orthotics to prevent recurrence. Corns may cause difficulty in completing daily activities. If this applies to you, it is suggested that you schedule an appointment with a podiatrist for an expert evaluation and effective relief.
If you have any concerns regarding your feet and ankles, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.