Toenail Fungus Is Common

Toenail fungus is a common nail infection. It is considered contagious, and most people will develop this foot condition at some point in their lives. It is noticeable by the yellow and thickened toenails, and in severe cases, the nail can become brittle and crumble. The fungus that causes this nail condition lives in warm and moist environments, including shower room floors, public swimming pools, and similar places. Effective prevention techniques can consist of refraining from sharing towels, shoes, and socks, in addition to wearing shoes that are made of breathable materials. People who have existing medical conditions, such as diabetes, psoriasis, or a weakened immune system may be prone to developing toenail fungus. If you see the beginning signs of this nail infection, it is strongly suggested that you consult with a podiatrist sooner rather than later who can discuss treatment options with you.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Athlete’s Foot in Seniors

If you are a senior citizen, you might have noticed that as you age, you become increasingly susceptible to poor foot health. As a result, a senior citizen might be at risk for developing foot conditions, such as athlete’s foot. Athlete’s foot is a particular kind of fungal infection that can result in a rash between the toes of the feet. Itching and redness can ensue. A senior might be prone to athlete’s foot because the elderly have a diminished ability to keep their feet clean and dry. Consequently, the fungus causing athlete’s foot can take hold in a senior. To prevent athlete’s foot, a senior can consider taking certain steps, such as regularly cleaning and drying the feet, applying a good moisturizer, and disinfecting the socks. If you are a senior looking to prevent athlete's foot, it is suggested that you contact a podiatrist for an appointment today.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Elderly Foot Care
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.
Why Live with Pain and Numbness in Your Feet?
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Corns Can Be Surprisingly Painful

A corn can be painful, despite its small size. They generally develop as a result of excess friction caused by the shoes worn, and the pain can alter the gait, or walking style. Common places for corns to develop can be the side of the pinky toe or on top of the toes. Prevention methods can include wearing shoes and socks that fit correctly, and it may help to moisturize the feet frequently. Many people find comfort in wearing insoles or heel pads in their shoes and soaking the corn in warm water at the end of the day. This may help to soften it and can make it easier to use a pumice stone that can file down small corns. If the corns are recurring, it is suggested that you consult with a podiatrist who can guide you toward additional prevention methods.
If you have any concerns regarding your feet and ankles, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Corns
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
Forefoot Pain
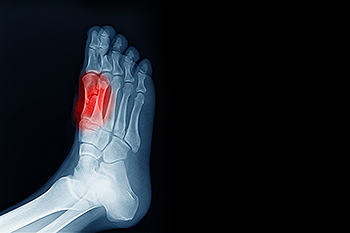
The forefoot is the front part of the foot that contains ligaments, tendons, muscles, nerves, blood vessels, metatarsal bones, and phalanges. The metatarsal bones are the five long bones between the toe bones, the hindfoot, and the midfoot. There are a variety of conditions that can lead to forefoot pain, including Morton’s neuroma, toe pain, and sesamoiditis. The focus here is on sesamoiditis. Most bones are connected to other bones at joints. Sesamoids are bones embedded in muscle and only connected to tendons. On the bottom of the foot, near the big toe, two small sesamoids help with weight bearing and raising the bones of the big toe. Sesamoiditis happens when these tendons become irritated and inflamed. This is common among runners and dancers. If you suffer from pain in your forefoot, it is suggested that you visit a podiatrist to determine the cause of the pain, whether it’s sesamoiditis, and how to treat it best.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Sesamoiditis
Sesamoiditis is a condition that affects the joint that is just behind the big toe in the area known as the ball of the foot. It is most common in younger people and people who have just begun an exercise program. Since the sesamoid bones are like a pulley controlling the big toe, they can rub against each other and cause a gradual onset of pain. Pain may also be caused by the inflammation of tendons surrounding the bones. If ignored, sesamoiditis can lead to other, more serious problems such as severe irritation and fractures of the bones.
The cause of sesamoiditis is sudden increase in activity. The ball of your foot acts as a springboard to help you lift off when you are jogging or running. Sudden increase in the use of these bones or the tendon that controls them can cause irritation. The tendon then begins to develop inflammation and the joint begins to swell. People with smaller, bonier feet or those with a high arch are typically more susceptible to this condition.
Sesamoiditis is fairly simple to diagnose since the symptoms have a gradual onset rather than a sudden impact. The symptoms begin with slight irritation around the joint shortly after the increase in activity. The discomfort eventually turns to pain with light swelling and possibly redness. Although redness or bruising are rare, this may be a symptom. After each session of exercising, the aggravated joint becomes more irritated and increases into a very intense throbbing.
Treatment for sesamoiditis can vary depending on the severity of the situation. However, treatment is almost always approached in a noninvasive way. For a case that is just beginning the doctor may recommend a very strict rest period that will limit the activity allowed on the joint. If you must be active, a recommendation for as modified shoe or insole, along with bandaging and immobilizing the big toe will be made to ensure that pressure is not placed on the joint. For severe cases, it is typically recommended that the joint and the big toe be completely immobilized to allow adequate time to heal. Ice and an over the counter anti-inflammatory may can help with the pain and discomfort while you are at rest.
When you return to your regular exercise activities, it is recommended that you use an insole that will allow even distribution of impact to your entire foot, rather than just the balls of your foot. This will prevent further aggravation of the injury.