Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Achilles Tendon Injury in Dancers
Dancers place significant strain on the Achilles tendon due to repetitive movements, jumps, and intense footwork. This can lead to inflammation, microtears, or even more severe injuries if not properly managed. Overuse, inadequate warm-ups, and wearing improper footwear increase the risk of injury. Strengthening the calf muscles and improving flexibility through targeted exercises can help reduce strain on the tendon. Proper technique, gradual intensity progression, and sufficient rest between training sessions are essential for injury prevention. Supportive footwear and using appropriate dance surfaces can also minimize stress on the Achilles tendon. Paying attention to early signs of discomfort, such as stiffness or pain, allows for timely intervention. If you have sustained an Achilles tendon injury from dancing, it is suggested that you promptly contact a podiatrist who can offer effective treatment solutions and prevention tips.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
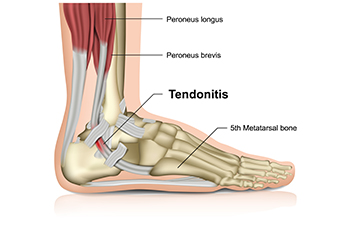
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.
Reduce Flat Feet Discomfort With Custom Orthotics

Flat feet? Rise above the discomfort with Custom Orthotics. Specifically designed to support the arch and align the foot, Custom Orthotics can be a game-changer for those with flat feet. They help in distributing weight evenly, preventing undue stress and potential pain. Walk, run, or stand with newfound confidence, knowing your feet have the support they've been missing. Want to explore the benefits of Custom Orthotics tailored for flat feet? Contact us today!
Definition and Risk Factors of Onychomycosis

Onychomycosis is a fungal infection that affects the toenails, causing discoloration, thickening, and brittleness. It develops when fungi invade the nail bed, thriving in warm and moist environments. Risk factors for fungal toenails include excessive sweating, prolonged exposure to damp conditions, and wearing tight or non-breathable footwear. Individuals with weakened immune systems, diabetes, or poor circulation are more susceptible to infection. Symptoms often begin with white or yellow spots on the nail, progressing to thickened, crumbly, or distorted nail surfaces. In some cases, the affected nails may become painful or emit an unpleasant odor. If you have the above symptoms, it is suggested that you promptly consult a podiatrist who can effectively treat toenail fungus, which may include prescribed medication.
For more information about treatment, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
Expert Prescription of Custom Orthotics

Prescribing custom orthotics is not as simple as taking a mold of the foot and inserting support. The feet are complex, and proper orthotics must consider biomechanics, muscle function, and overall alignment. While orthotics help redistribute pressure and correct imbalances, they should also work with the body’s natural movement, not replace it. If orthotics do all the work, the muscles they support can weaken over time. That is why a podiatrist carefully evaluates foot structure, gait, and strength before prescribing orthotics. They ensure the right balance of support and engagement, helping muscles function properly while reducing pain. The wrong orthotics can actually worsen issues instead of improving them. If you are experiencing foot pain and considering orthotics, it is suggested that you see a podiatrist to ensure that if they are prescribed, they will enhance movement, support healing, and keep your feet strong and aligned.
Experience a transformative solution to heel pain and foot pain through the personalized benefits of custom orthotics and shoe inserts. If you’re grappling with the persistent agony of plantar fasciitis, these customized inserts are designed to alleviate the strain on the plantar fascia, providing targeted relief. Engineered to adapt to your unique foot anatomy, custom orthotics tackle not only plantar fasciitis but also general foot and heel pain, offering unparalleled support and comfort. Don’t let every step be a reminder of discomfort; step into a world of tailored well-being. Say farewell to the limitations imposed by heel pain and embrace the freedom of pain-free mobility. Invest in your foot health and redefine your daily stride with the transformative power of custom orthotics and shoe inserts, ensuring each step is a step towards lasting comfort.
If you have any questions please contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Understanding Foot Puncture Wounds

A foot puncture wound is a deep injury caused by a sharp object piercing the skin and underlying tissues. Unlike surface cuts, these wounds can introduce bacteria deep into the foot, increasing the risk of infection. Common causes include stepping on nails, glass, splinters, or sharp metal objects, often in outdoor or workplace settings. Symptoms may include immediate pain, swelling, redness, and bleeding at the injury site. If an infection develops, additional signs such as warmth, pus, or increased pain may occur. In some cases, a foreign object may remain embedded in the wound, leading to prolonged discomfort. If you have a puncture wound on your foot, it is suggested that you promptly consult a podiatrist who can offer appropriate treatment remedies.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.