The Impact of Flip-Flops on Foot Biomechanics and Gait

Flip-flops, while popular for their convenience and comfort, can negatively affect foot biomechanics and gait. These minimalistic shoes offer limited support and cushioning, leading to poor alignment of the foot and increased stress on the muscles and joints. The lack of arch support and cushioning can cause abnormal gait patterns, such as overpronation or supination, which may result in foot pain or discomfort. Additionally, the loose fit of flip-flops requires constant gripping with the toes to keep them on, which can strain the foot muscles and contribute to imbalance. Over time, frequent use of flip-flops may worsen existing foot problems or lead to new issues such as plantar fasciitis or metatarsalgia. If you have developed one or more foot conditions from wearing flip-flops, it is suggested that you consult a podiatrist for effective treatment.
Flip-flops are not always the best choice of footwear. If you have any concerns about your feet or ankles, contact Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
When the weather starts warming up, people enjoy wearing flip-flops. Flip-flops are comfortable, stylish, and easy to slip on and off; they're perfect for any summer beach goer. However, these shoes can cause harm to the feet.
How Can Flip-Flops Affect Me Long-Term?
- Ankle problems
- Hip problems
- Lower back problems
- Pain in the balls of the feet
- Problems with foot arches
- Changes in the way you walk
Are There Injuries Associated with Flip-Flops?
Yes. Since flip-flops are relatively weak and do not provide the same amount of support as sneakers, people who wear flip-flops regularly are more susceptible to injuries. On top of that, the open nature of the shoe makes your feet more prone to other problems, such as cuts and even infections. Common injuries and ailments include:
- Sprained ankles
- Blisters
- Infections
- Cuts and Scrapes
I like Wearing Flip-Flops. Are There Safe Alternatives?
When buying flip-flops, try to find ones that have sturdy soles and that are made of high-quality materials that will support for your feet. These flip-flops will cost more but will also last longer as a result.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flip Flops and Your Feet
When the weather heats up, you may want to start wearing flip-flops. However, it has been proven that these are not the ideal shoes in terms of preserving the health of your feet.
Flip flops are known to expose your feet to different types of bacteria and fungal infections. When you wear your flip flops in public, you are exposing them to staphylococcus which is a skin-irritating bacterium. Athlete’s foot is also highly contagious and can be spread when you walk around nearly-barefoot.
Another harmful effect of wearing flip-flops is that they develop blisters on the feet. This is because the thin strap rubs against the skin with each step taken. Unfortunately, when blisters pop, they cause you to be more vulnerable to pathogens you pick up by having your feet exposed.
These shoes may also cause “shooting pains”. If you have flat feet, you need arch support to keep your knees, hips, and back in alignment. If you wear flat shoes, your joints are forced to compensate which can cause injuries throughout the body.
If you constantly wear flip-flops, you should avoid doing so as they can lead to many problems for your feet. If you are experiencing any of these foot issues, you should seek help from a podiatrist right away.
Bypass Bunion Surgery with Custom Orthotics

Considering bunion surgery? Think again. Custom Orthotics offer a non-surgical approach to reduce pain and restore foot function. Customized to your foot's structure, they realign and redistribute pressure, alleviating bunion discomfort. Experience the freedom of movement without the downtime and risks of surgery. Contact our office to make an appointment.
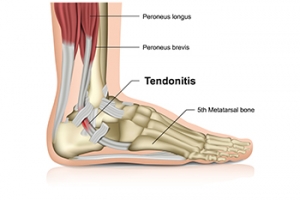
Facts About the Achilles Tendon and Potential Injuries
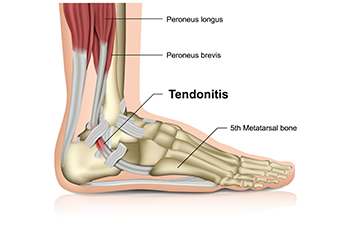
The Achilles tendon, the largest tendon in the body, connects the calf muscles to the heel bone, playing a vital role in walking, running, and jumping by facilitating the movement of the foot. Achilles tendon injuries often result from overuse, excessive strain, or sudden increases in physical activity. Causes include repetitive stress from activities like running or jumping, improper footwear, or muscle imbalances. People prone to these injuries include athletes, especially those involved in sports requiring quick changes in direction, and anyone who suddenly intensifies their exercise routines without proper conditioning. Other risk factors include age-related tendon degeneration and pre-existing conditions like diabetes or arthritis. Achilles tendon injuries can cause severe pain and discomfort. If you have sustained this type of injury, it is suggested that you promptly consult a podiatrist who can effectively treat and manage this condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Anas Khoury, DPM of North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Orthotics for Diabetic Foot

Orthotics can play an important role in managing diabetic foot care, offering essential support and protection. Diabetic feet are more prone to complications due to poor circulation and nerve damage, which can lead to foot deformities, ulcers, and increased risk of infection. These issues make it vital to maintain proper foot alignment and reduce pressure on vulnerable areas. Custom orthotics are specialized shoe inserts designed to provide support, correct foot mechanics, and distribute pressure evenly across the foot. For people with diabetes, this can prevent the formation of ulcers by reducing friction and pressure on sensitive areas, thereby minimizing the risk of wounds that can lead to serious complications. Orthotics also help in managing foot deformities common in diabetes, such as Charcot foot, by providing stability and preventing further damage. Regular use of orthotics, coupled with proper foot care, can significantly improve foot health and reduce the risk of severe complications in diabetic patients. If you are a diabetic, it is strongly suggested that you include a podiatrist on your healthcare team to inspect your feet regularly, find areas in need of treatment, and provide injury prevention tips.
If you’re experiencing foot discomfort, have a history of foot and ankle injuries, or are interested in exploring Custom orthotics, don’t hesitate to contact Anas Khoury, DPM at North Eastern Foot & Ankle Specialists. Our doctor is dedicated to offering the care required to help you remain pain-free and stay on your feet.
What are Custom Orthotics?
Custom orthotics refer to custom inserts designed for placement in different shoe types, including athletic and formal footwear, with the purpose of alleviating a spectrum of foot-related problems such as flat feet, heel pain, and overall foot discomfort. These inserts are instrumental in providing relief and comfort for a diverse range of foot conditions, including heel pain, and can also act as a proactive approach to injury prevention.
Medical Grade Shoe Inserts:
A diverse array of shoe inserts is available for addressing foot pain, heel discomfort, and minor issues. For instance, you can place arch supports in your shoes to rectify overarched or flat feet, and gel and cushioned insoles are frequently chosen for the comfort and relief they provide from foot and heel pain by reducing pressure.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Facts About High Ankle Sprains

A high ankle sprain, also known as a syndesmotic sprain, involves injury to the ligaments that connect the two bones of the lower leg known as the tibia and fibula, above the ankle joint. This type of sprain is distinct from a regular ankle sprain, which affects the ligaments surrounding the ankle joint itself. Symptoms of a high ankle sprain typically include pain above the ankle, swelling, and difficulty bearing weight on the affected leg. The injury often results from activities that involve twisting or turning movements, such as in sports or accidents. Causes may include sudden, forceful rotations of the foot or direct trauma to the lower leg. If you have sprained your ankle, it is suggested that you visit a podiatrist as quickly as possible who can accurately diagnose the type of sprain, and treat it accordingly.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Anas Khoury, DPM from North Eastern Foot & Ankle Specialists. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Passaic, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.